In The Appeals Process Calendar Days Are Considered
In The Appeals Process Calendar Days Are Considered - Appeal and claim dispute form. Web tips for a timely review. (some part a only) notice of discharge or service termination. A(n) ________ claim status category code is an acknowledgment that the claim has been received. Web verified answer for the question: In order to appeal to omha, you must. Within 180 calendar days of the. The appeals process begins at level 1. This section covers only omha’s role at level 3 of the appeals process. [revised] 2019 authorization and filing. Anab must receive the appeal within 30 calendar days of notification of the accreditation decision that is the. 180 days a first level provider payment review must be initiated within 180 calendar days from the date of the initial payment or denial decision from cigna. Web according to aetna's published guidelines, what is the timeframe for filing an appeal? Web. This section covers only omha’s role at level 3 of the appeals process. Web an ma plan is required to provide enrollees with information regarding the appeals process as part of the plan materials. Within 180 calendar days of the. Web you can submit an appeal using anab’s appeal form. Appeal and claim dispute form. Web in the appeals process, calendar days are considered all days, including weekends. Web according to aetna's published guidelines, what is the timeframe for filing an appeal? Appeal and claim dispute form. Web under the federal rules of appellate procedure, your notice of appeal must be received by the district court that heard your case or imposed the sentence within. Web by law, you must file your appeal within 10 calendar days of the mailing date listed on the determination or the appeal tribunal decision. Web up to 60 days after you get the qic decision notice or after the expiration of the qic reconsideration time frame, if you don’t get a decision. Web in the appeals process, calendar days. Web up to 60 days after you get the qic decision notice or after the expiration of the qic reconsideration time frame, if you don’t get a decision. (some part a only) notice of discharge or service termination. Within 180 calendar days of the. 180 days a first level provider payment review must be initiated within 180 calendar days from. The appeals process begins at level 1. In the appeals process, when calculating deadlines, 'calendar days' include all days,. Appeal and claim dispute form. Within 180 calendar days of the. Web up to 60 days after you get the qic decision notice or after the expiration of the qic reconsideration time frame, if you don’t get a decision. Web up to 60 days after you get the qic decision notice or after the expiration of the qic reconsideration time frame, if you don’t get a decision. Web to request an expedited reconsideration at level 2, you must submit a request to the appropriate qic no later than noon of the calendar day following your notification of the. Appeal. This section covers only omha’s role at level 3 of the appeals process. (some part a only) notice of discharge or service termination. Web the deadline to file an appeal is 30 calendar days after receipt of that decision or notification by the lender of the decision, whichever comes first. Web up to 60 days after you get the qic. Web an ma plan is required to provide enrollees with information regarding the appeals process as part of the plan materials. 180 days a first level provider payment review must be initiated within 180 calendar days from the date of the initial payment or denial decision from cigna. Web verified answer for the question: Claim dispute (formal dispute) 60 calendar. Within 180 calendar days of the. A(n) ________ claim status category code is an acknowledgment that the claim has been received. Anab must receive the appeal within 30 calendar days of notification of the accreditation decision that is the. Web under the federal rules of appellate procedure, your notice of appeal must be received by the district court that heard. In order to appeal to omha, you must. Web in the appeals process, calendar days are considered all days, including weekends. For cys 2022 and 2023, the. In the appeals process, when calculating deadlines, 'calendar days' include all days,. 180 days a first level provider payment review must be initiated within 180 calendar days from the date of the initial payment or denial decision from cigna. Within 60 calendar days of the initial claim decision b. Web medicare administrative contractor (mac) initial determination. Web a member’s appeal of a decision about authorizing healthcare or terminating coverage of a service must generally be resolved by meridian within 15 calendar days if. This section covers only omha’s role at level 3 of the appeals process. [solved] in the appeals process, calendar days are considered a) all days, including weekends. If the 10th day falls on a weekend or. Claim dispute (formal dispute) 60 calendar days from the written determination of the claim. Web according to aetna's published guidelines, what is the timeframe for filing an appeal? Web by law, you must file your appeal within 10 calendar days of the mailing date listed on the determination or the appeal tribunal decision. The appeals process begins at level 1. Web up to 60 days after you get the qic decision notice or after the expiration of the qic reconsideration time frame, if you don’t get a decision.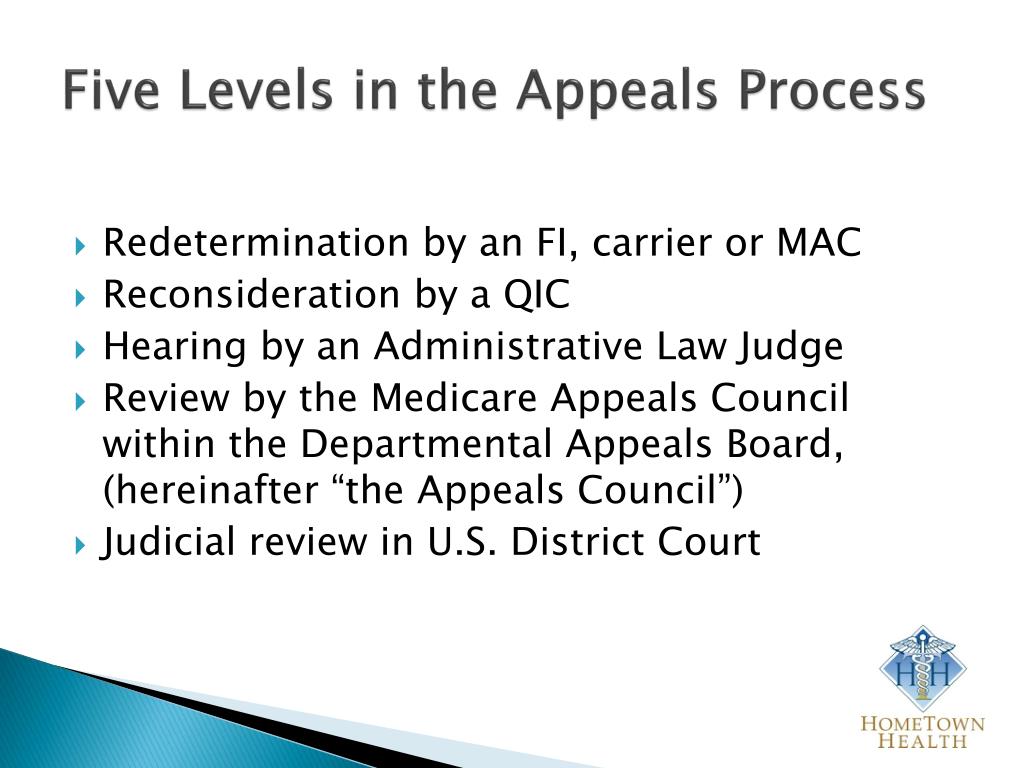
PPT THE MEDICARE APPEALS PROCESS PowerPoint Presentation, free

What Is The Medicare Appeals Process? REMEDIGAP
Appeals Process

Florida & Federal Appeals Process Appellate Court Structure Bushell
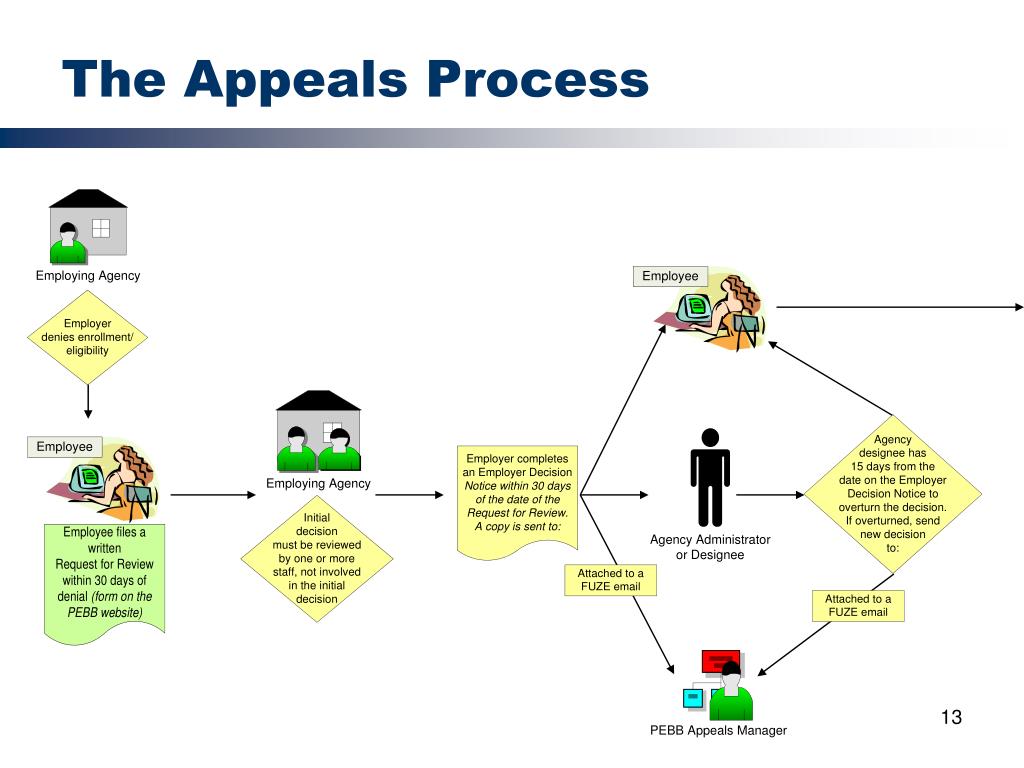
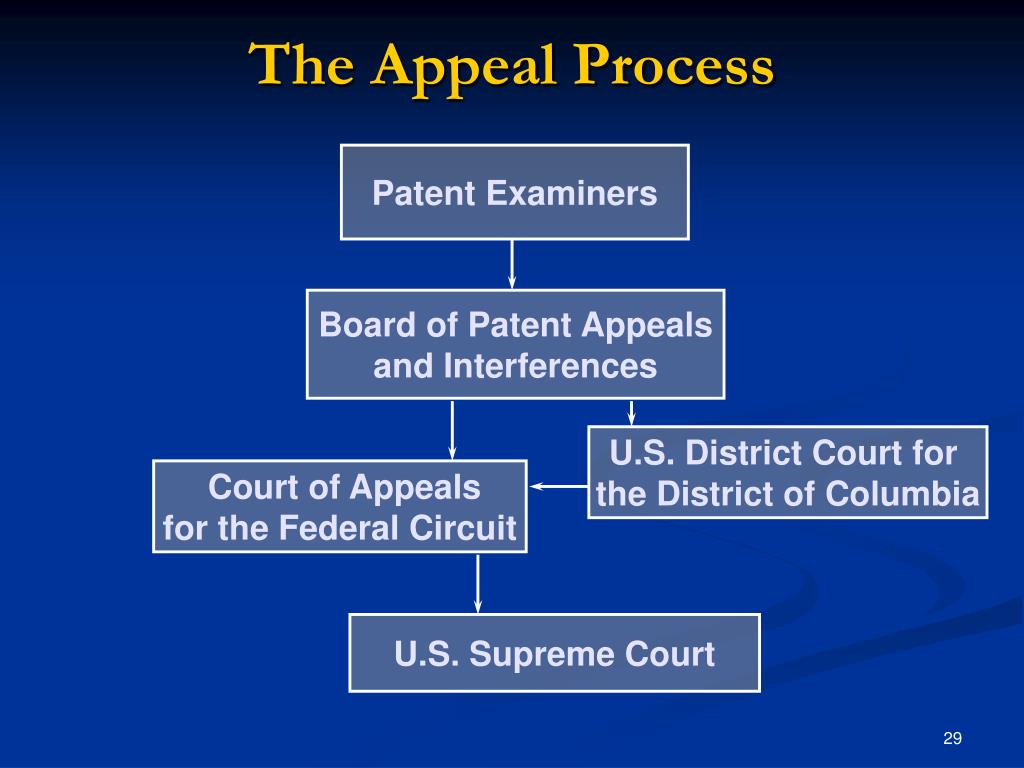
PPT Appeals Process PowerPoint Presentation, free download ID4128068
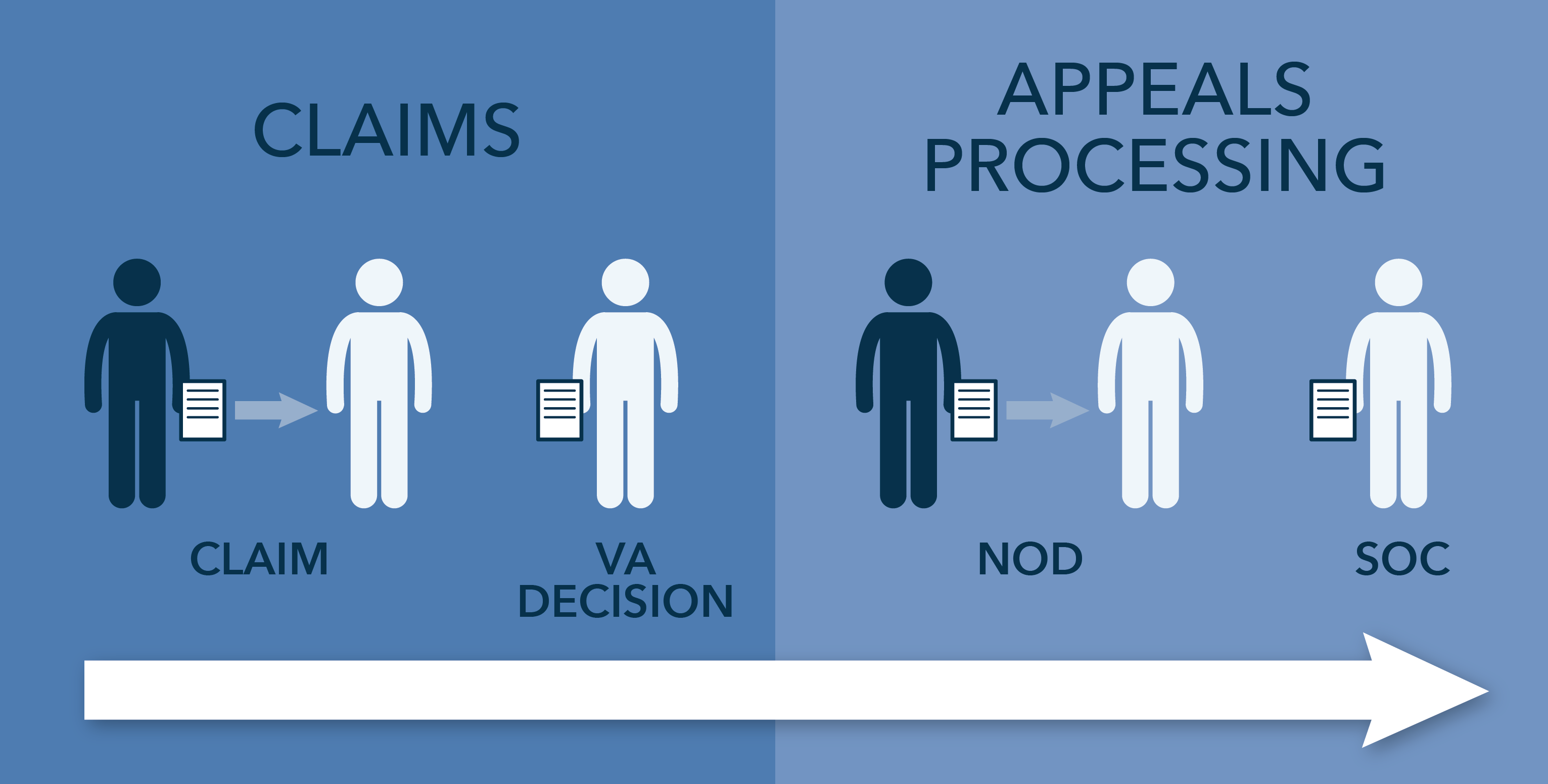
The appeals process Appeals at the regional office level VA News
Appeals Process
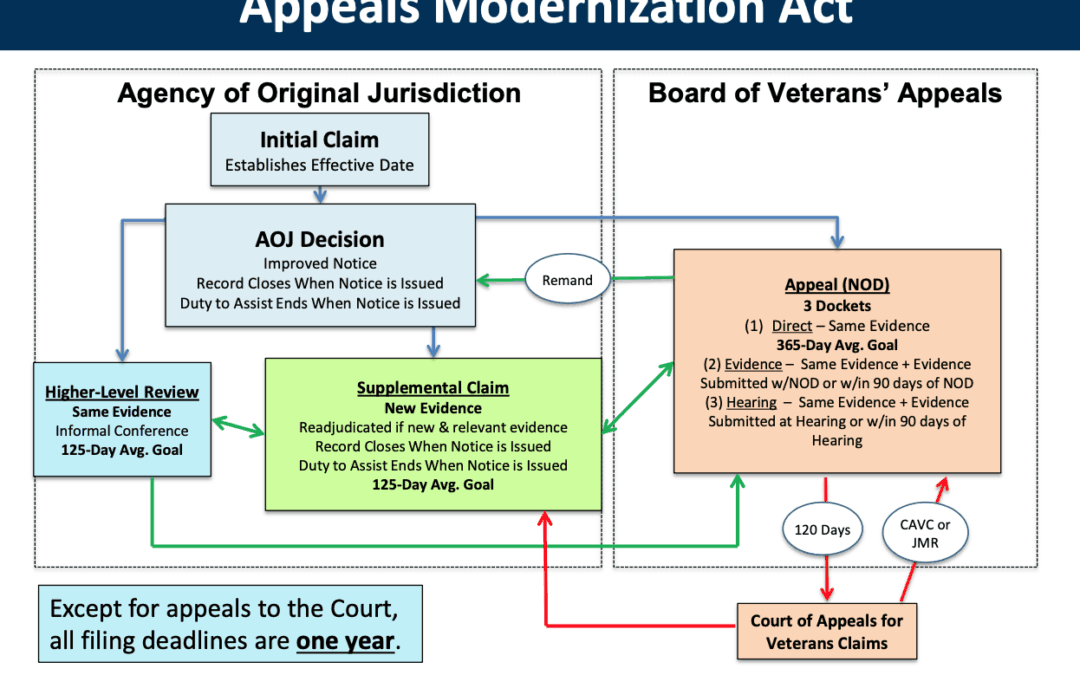
The VA's Modernized Appeal (AMA) Process Veterans Law Blog®
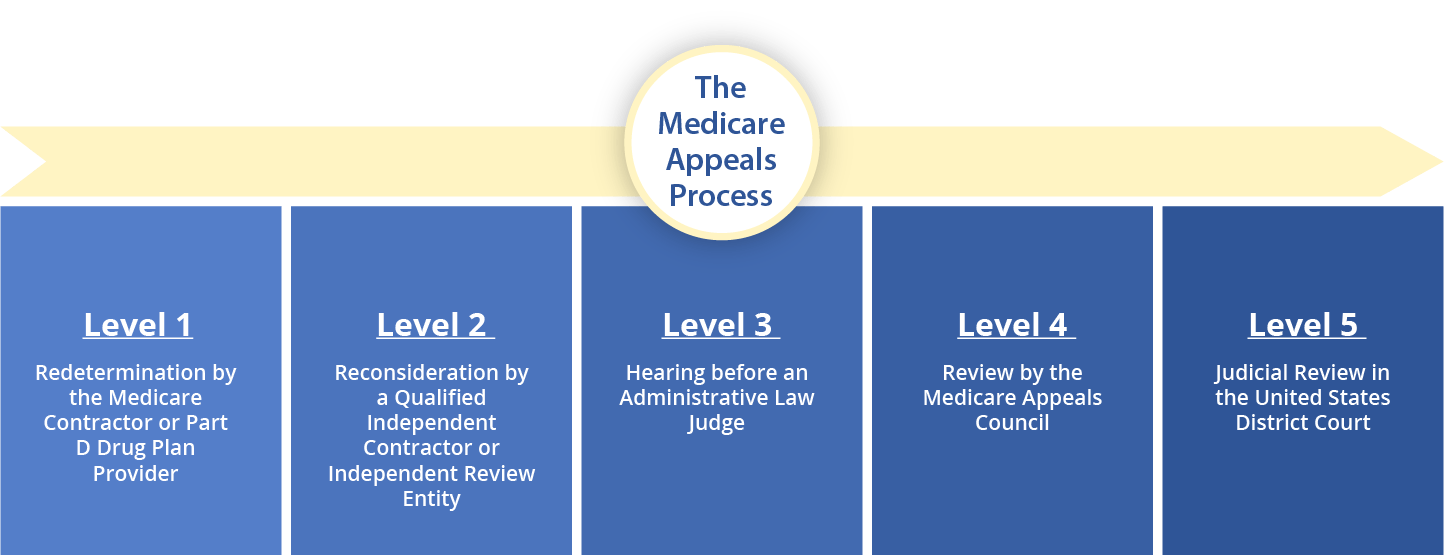
Medicare Appeals MSA MSA Meds
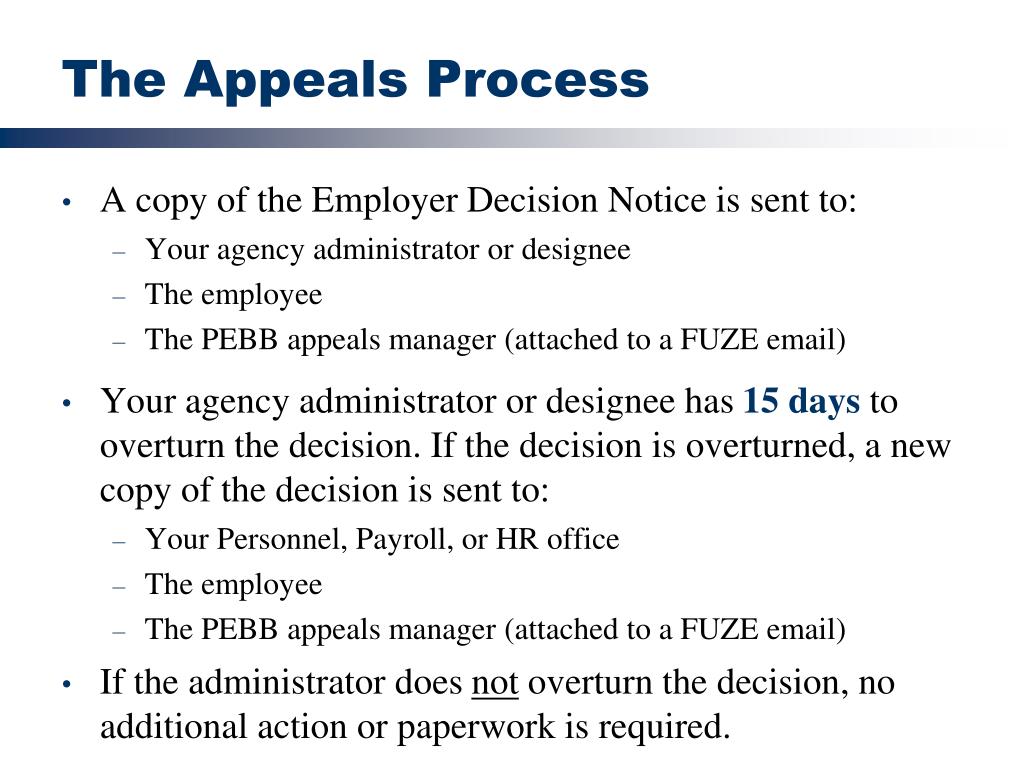
PPT Appeals Process PowerPoint Presentation, free download ID4128068
Web The Deadline To File An Appeal Is 30 Calendar Days After Receipt Of That Decision Or Notification By The Lender Of The Decision, Whichever Comes First.
[Revised] 2019 Authorization And Filing.
Web Tips For A Timely Review.
Within 180 Calendar Days Of The.
Related Post: